Short- and long-term outcomes for ethnic minorities in the United States after liver transplantation: Factors associated with graft failure
David M. O'Sullivan1, Heather L. Kutzler2, Caroline L. Rochon2,3, Glyn Morgan2,3, Michael Einstein2, Eva Sotil2, Colin Swales2, Patricia A. Sheiner2,3, Oscar Serrano2,3.
1Research Administration, Hartford Hospital, Hartford, CT, United States; 2Transplant Program, Hartford Hospital, Hartford, CT, United States; 3Surgery, University of Connecticut School of Medicine, Farmington, CT, United States
Purpose: Despite having greater severity of alcoholic liver disease, higher incidence of hepatocellular carcinoma and non-alcoholic fatty liver disease, and higher mortality from hepatitis B and C infection, ethnic minorities in the United States (U.S.) have a lower number of referrals for liver transplantation (LT) compared to non-Hispanic Whites (NHW). We sought to identify factors associated with graft failure and how they differ by race/ethnicity.
Methodology: We evaluated data from the U.S. Scientific Registry of Transplant Recipients (SRTR) of all adult LT recipients between 1999 and 2014 and compared outcomes by race or ethnicity: Hispanic, NHW, and non-Hispanic Blacks (NHB). We assessed 1- and 5-year patient survival (PS) and death-censored graft survival (DCGS). Donor and recipient characteristics controlled for included: living or deceased donor, brain-death or cardiac-death donor (DCD), recipient age, BMI, primary disease, MELD score, re-transplant status, graft rejection, and cold ischemia time (CIT). Cox regression analysis was used with an alpha level of 0.05.
Results: During these 15 years, 82,654 (63,557 NHW, 8,024 NHB, and 11,073 Hispanic) adult LT recipients were performed in the U.S. One-year PS for NHW, NHB, and Hispanics was 88.2%, 85.7%, and 88.7%, respectively; one-year DCGS was 95.8%, 95.3%, and 95.6%, respectively. Five-year PS for NHW, NHB, and Hispanics was 76.5%, 70.8%, and 78.1%, respectively; five-year DCGS was 94.3%, 92.8%, and 94.1%, respectively. Compared to NHW, NHB PS and DCGS were significantly lower at 1 year (p<0.001 and p=0.03, respectively) and 5 years (p<0.001 for both). Conversely, Hispanic PS was significantly higher at 5 years (p<0.001) than NHW. 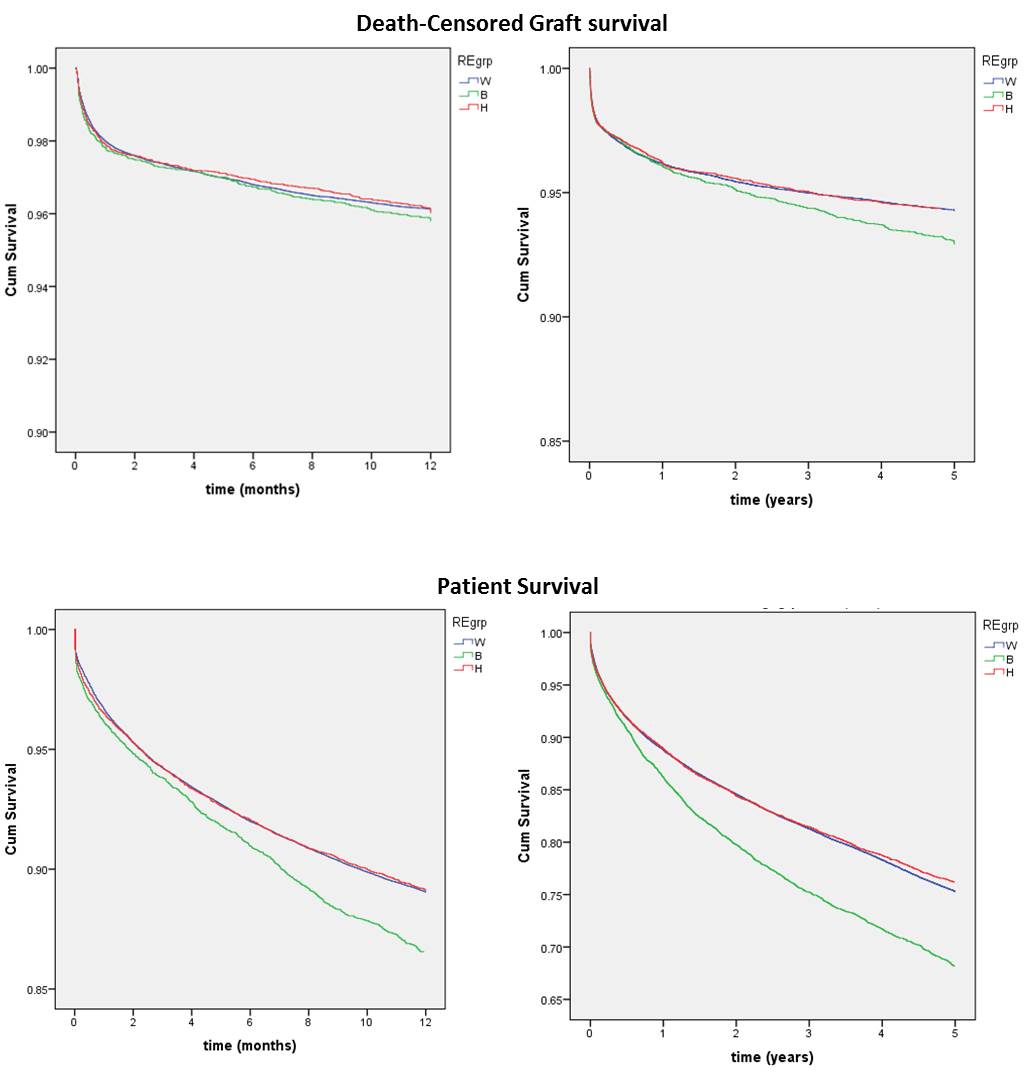
Multivariate analysis of one-year graft loss showed that older recipient age (HR 1.011, 95% CI 1.009-1.013), re-transplant status (1.971, 1.851-2.099), longer CIT (1.035, 1.030-1.040), graft rejection (1.293, 1.194-1.400) and a DCD donor (1.500, 1.381-1.629) were predictive of graft loss.
Conclusion: We show differences in short- and long-term outcomes after LT for minority patients and have identified risk factors associated with graft loss. Further research is necessary to improve our understanding of ethnicity and race and how they affect outcomes after LT.