Combined heart-kidney transplantation: single center experience
Angela Sickels1, Brianna Ruch1, Gaurav Gupta1, Adrian Cotterell1, Chandra Bhati1, Seung Lee1, Aamir Khan1, Marlon Levy1, Vigneshwar Kasirajan2, Keyur Shah2, Amit Sharma1.
1Hume-Lee Transplant Center, Virginia Commonwealth University, Richmond, VA, United States; 2Pauley Heart Center, Virginia Commonwealth University, Richmond, VA, United States
Introduction: Combined heart and kidney transplant (CHKT) was first described in 1978 (1). Although CHKT is increasing in frequency, there are still no guidelines to establish the indications, contraindications and sequence for this surgical procedure. Concomitant heart failure and renal insufficiency warrants consideration for CHKT when the estimated GFR is < 30-40 mL/min per m2, without necessitating dialysis dependence (2). We present our single center experience with CHKT.
Methods: Data were prospectively collected and retrospectively reviewed in the medical records of all patients that underwent CHKT at our center between 09/2015 and 05/2019. Both organs were taken from the same deceased donor and transplanted as ‘combined’ rather than ‘staged’ procedures. Continuous variables are expressed using mean (± standard deviation) or median (range). Categorical variables are presented as counts and proportions.
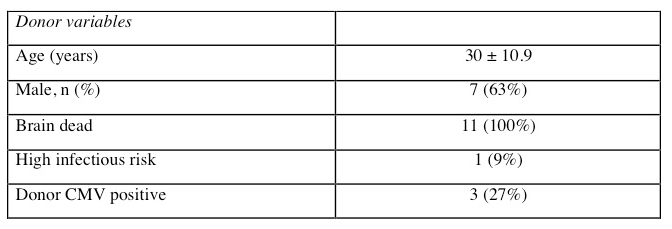
Results and Discussion: All organs were procured from brain dead donors (mean age 30 ± 10.9 years) and transplanted in to recipients with mean age of 49.5 ± 14.6 years.
Nine out 11 recipients (81.8%) had mechanical circulatory support. Two patients (18%) had a previous heart transplants. Five out of 11 (45%) patients had diabetes and were on hemodialysis prior to CHKT. The mean GFR pre-transplant was 21.27 ± 31.81 ml/min/m2
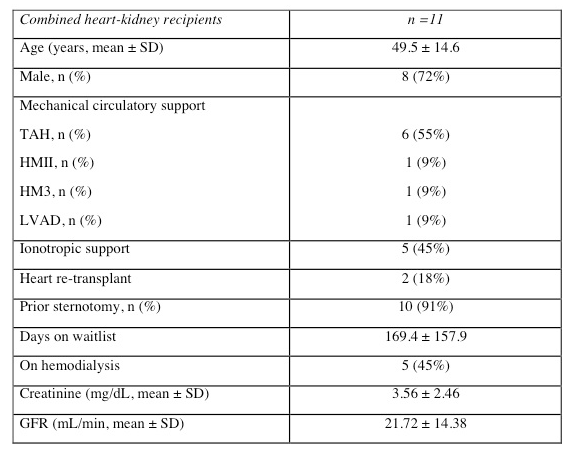
A majority (91%) had a previous sternotomy and the heart was transplanted using the bicaval orthotopic technique. The kidney was transplanted to the external iliac vessels (91%). All patients received induction therapy either with basiliximab (73%) or thymoglobulin (27%).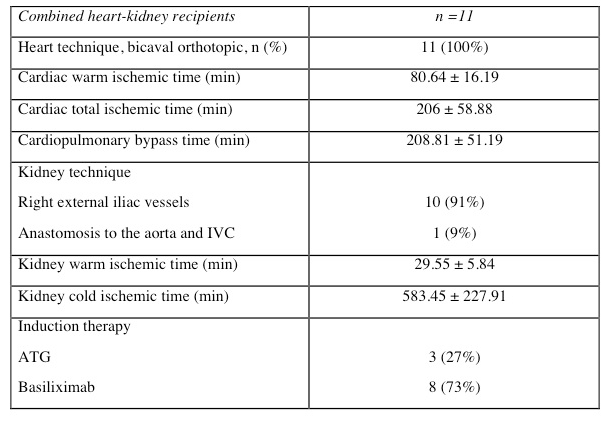
The 1-year patient and graft survival for both organs was 100% with a median follow up of 18 months (range 8-46). Four out of 11 (45%) patients had delayed graft function (DGF). All patients with DGF had history of pre-transplant diabetes and 60% were on dialysis pre-transplant. Four patients had rejection episodes: 2 had concomitant heart (both grade 1R) and kidney (one acute antibody mediated and one T-cell mediated) rejection and 1 patient each had isolated heart and kidney rejections. Two of these patients had received thymoglobulin while the other two had basiliximab induction. However, all patients had freedom from rejections ≥grade 2. Five patients (55%) had seven infectious episodes: pneumonia (2), urinary tract infection (2), mediastinitis (1), HSV esophagitis (1), C. difficile (1).

Conclusions: Combined heart and kidney transplantation is safe and feasible, with excellent outcomes for both the allografts and should be offered to patients with advanced heart failure and renal insufficiency. Immunosuppressive protocols should be tailored to minimize the risk of infectious complications while avoiding rejection episodes. The reasons for delayed graft function after combined heart and kidney transplantation need further evaluation.
[1] Norman JC, Brook MI, Cooley DA, Klima T, Kahan BD, Frazier OH et al. Lancet.1978;1:1125–7.
[2] Habib PJ, Patel PC, Hodge D et al. J Heart Lung Transplant. 2016; 35:1471–1479.
There are no comments yet...