Short recipient warm ischemia time improves graft survival in deceased donor liver transplantation: 20-year experience of liver transplantation
Toshihiro Kitajima1, Shunji Nagai1, Abbas Al-Kurd1, Khortnal Delvecchio1, Sirisha Yeddula1, Michael Rizzari1, Atsushi Yoshida1, Marwan Abouljoud1, Kelly Collins1.
1Transplant and Hepatobiliary Surgery, Henry Ford Hospital, Detroit, MI, United States
Background: Although the correlation between warm ischemia time (WIT) and the outcomes liver transplantation has been extensively studied, few investigations have focused on the effect of recipient short WIT on outcomes of liver transplantation in donation after brain-death (DBD) donors.
Methods: Our institutional Transplant Surgery Database was retrospectively queried to identify patients who underwent primary DBD liver transplantation between 2000 and 2019. Patients were divided according to recipient WIT (≤30 [Group A], 31-40 [Group B], 41-50 [Group C] and >50 minutes [Group D]), and short- and long-term graft survival was assessed. Graft survival was compared by a log-rank test and risk of graft loss was assess using a Cox regression multivariate model.
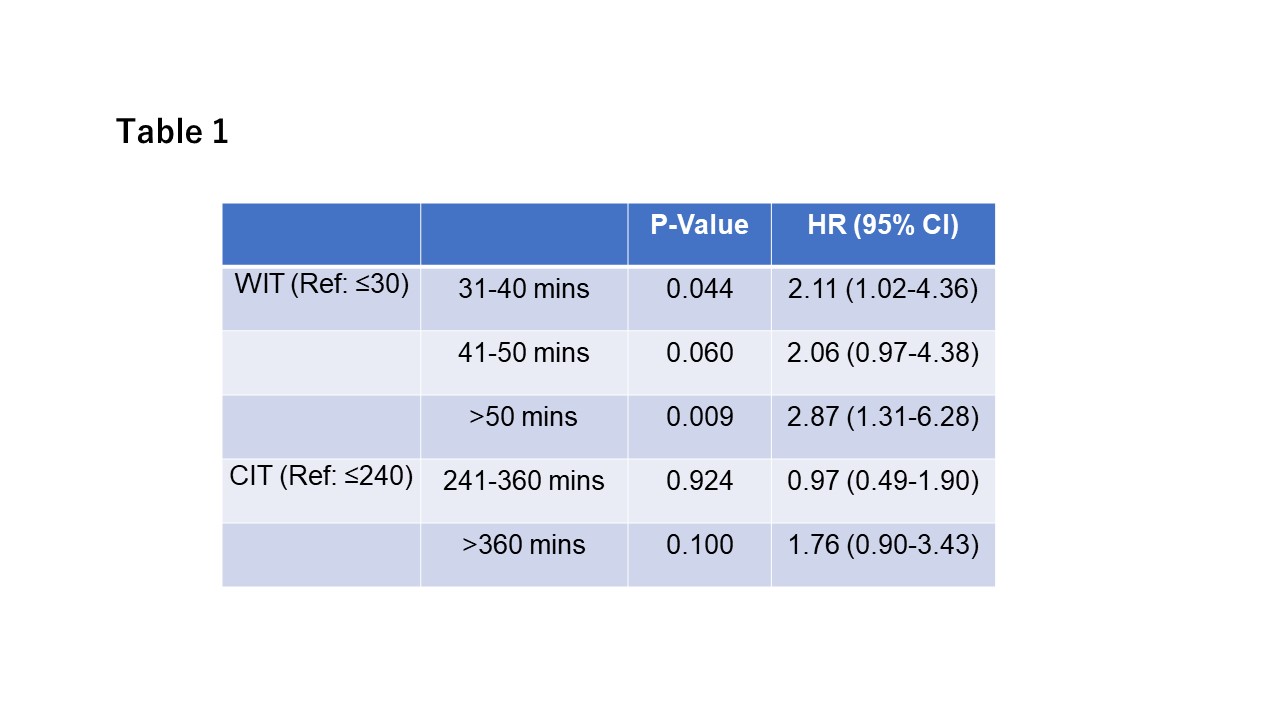
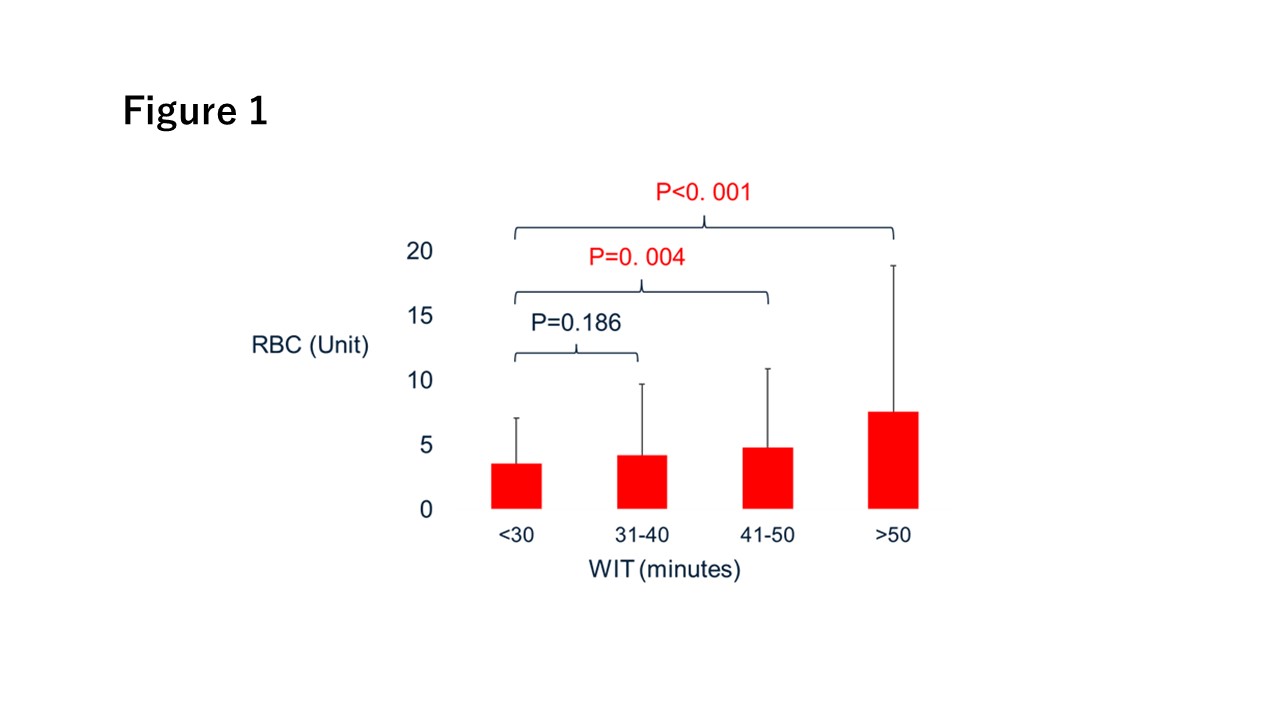
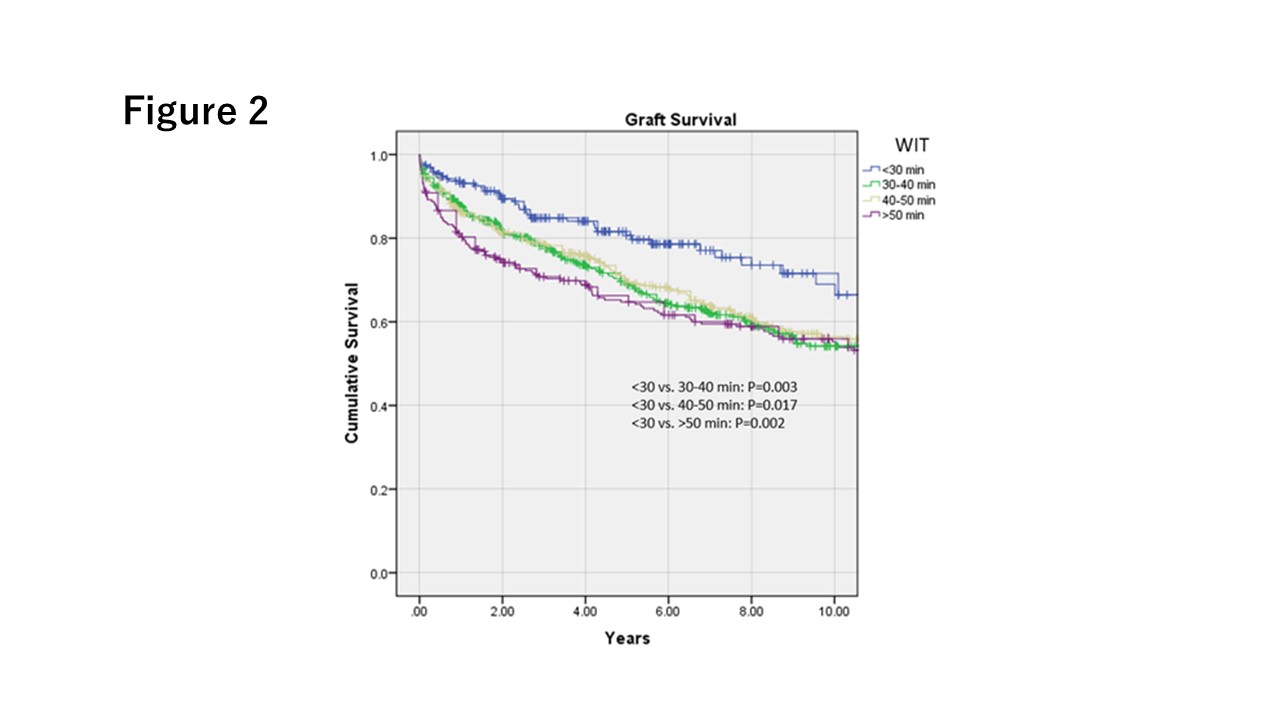
Results: During the study period, 1,256 DBD liver transplants were performed. These patients had a mean age of 55.1±9.7 and 65.7% were males. The mean pretransplant MELD score was 28.8±8.9. Recipient WIT was ≤30 minutes in 195 patients (15.5%), 30 – 40 minutes in 468 patients (37.3%), 40 – 50 minutes in 353 patients (28.1%) and >50 minutes in 240 patients (19.1%). Mean age was older (P=0.037) in Group A, and MELD score at liver transplantation was similar between 4 groups (P=0.137). The amount of red blood cell transfusion was significantly lower in Group A than in Group C (P=0.004) and Group D (P<0.001, Figure 1), and the requirement of cryoprecipitate, fresh frozen plasma, and platelets transfusion were also significantly lower in Group A (P<0.001). Group A showed better graft survival than others throughout 10-year follow-up period (Figure 2). One-year survival in Group A was significantly better than in Group B (93.3% vs. 87.7%, respectively, P=0.04), Group C (93.3% vs. 86.4%, P=0.019) and Group D (93.3% vs. 80.8%, P<0.001). Upon multivariate analysis, with adjustment for donor, recipient, and operative factors and year of transplantation, WIT≤30 minutes remained a significant predictor of superior graft survival when compared to the other groups (Table 1). Cold ischemia time was associated with graft survival in univariate analysis, but did not remain as an independent factor.
Conclusion: Shorter recipient WIT in DBD liver transplants is associated with significantly lower amount of intra-operative blood transfusion and superior short and long-term graft survival. It is important to attempt to keep WIT within 30 minutes when feasible.