Pulsatile perfusion in pediatric kidney transplantation
Malcolm MacConmara1, Ahmad Mashmoushi1, Dev Desai1, Parsia Vagefi1, Christine Hwang1.
1Surgery, UT Southwestern Medical Center, Dallas, TX, United States
Introduction: Pulsatile perfusion of deceased donor kidneys is commonly practiced in adult kidney transplantation. We examined the practice of pulsatile perfusion in pediatric patients undergoing kidney transplantation and compared outcomes from preservation using pulsatile perfusion (PUMP) and static cold storage (COLD) in pediatric recipients.
Methods: The UNOS database was used to determine outcomes in all pediatric kidney recipients (<18 years) who were transplanted between 1994—2018. Living donor and multi-organ transplant recipients were excluded. Patients were divided according to preservation method into PUMP or COLD groups. Donor and recipient demographic data were examined, as were survival and outcomes. A p-value of <0.05 was considered to be significant.
Results: There were 10,045 pediatric kidney transplants performed during the study period, of which 1,619 were PUMP (16.1%) and 8,426 were COLD (83.9%). PUMP donors were significantly younger (22.7 vs. 23.8 years), had a higher KDPI (22.4% vs. 19.7%), longer cold storage time (18.8 vs. 14.1 hours), more frequent donation after cardiac death (DCD) donor status (12.9% vs. 1.3%), and more likely to be an increased risk of disease (IRD) transmission donor (9.1% vs. 4.8%). PUMP kidneys were also more likely to have been biopsied (18.1% vs. 3.3%). There were no differences in donor creatinine (0.99 vs. 0.96 mg/dL). Recipients of PUMP kidneys were significantly older (12.0 vs. 11.6 years), had a shorter wait time (287.7 vs. 320.2 days), and greater HLA mismatch (4.5 vs. 4.3). There were no differences in BMI, initial or final cPRA, length of stay, or serum creatinine at the time of discharge (1.42 vs. 1.42 mg/dL). No differences in allograft survival at 10 years were noted between PUMP and COLD groups (Figure 1). Additionally, delayed graft function (DGF) occurrence (8.5% vs. 12.5%, p<0.05) and rejection rate in the initial 12 months post transplant (11.5% vs. 13.8%) were significantly lower in the PUMP group compared with the COLD group.
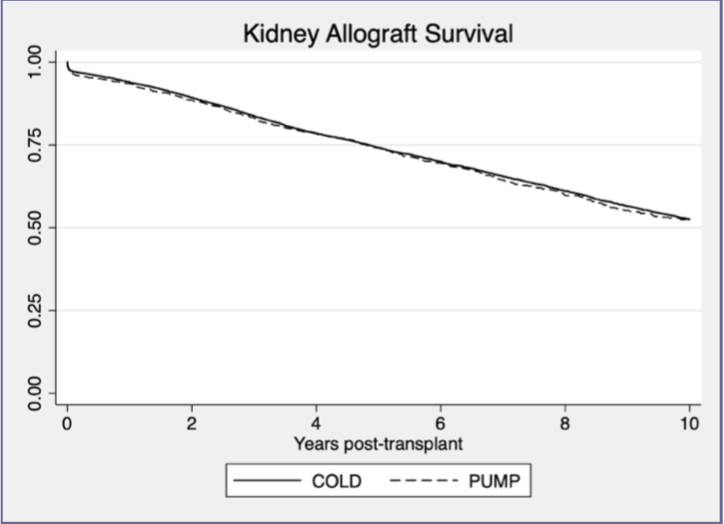
Conclusions: Despite multiple unfavorable characteristics noted in PUMP donors, recipients of these kidneys have no difference in allograft survival and have a lower DGF rate. These data support the utilization of pulsatile perfusion during the evaluation of higher risk pediatric kidney donors and a possible role in improving outcomes for pediatric kidney transplantation.