
Missed opportunities for organ donation from potential donors with primary brain tumours in Australia; cohort study 2010-2015
Imogen Kate Thomson1, James Hedley1, Brenda Rosales1, Patrick Kelly1, Kate Wyburn1,2, Angela Webster1,3.
1Sydney School of Public Health, Faculty of Health and Medicine, University of Sydney, Sydney, Australia; 2Renal Department, Royal Prince Alfred Hospital, Sydney, Australia; 3Centre for Transplant and Renal Research, Westmead Hospital, Sydney, Australia
Centre for Organ Donation Excellence.
Aims: The critical shortage of donor organs represents a global challenge necessitating consideration of all potential safe donors. Most primary brain tumours (PBTs) are not a contraindication to organ donation as risk of tumour transmission to a transplant recipient is low. However, uncertainty regarding transmission risk and biovigilance may result in some referrals being overlooked due to the presence of PBT. We aimed to describe referrals with PBTs in New South Wales (NSW) Australia, identify any transmission events from PBT donors, and highlight potential missed opportunities for donation among organ donor referrals declined due to the presence of PBT.
Methods: We undertook a retrospective population-based cohort study in NSW Australia, utilising the Safety and Biovigilance in Organ Donation (SAFEBOD) public health register linking donors’ and recipients’ records in NSW Organ and Tissue Donation Service datasets, NSW Ministry of Health datasets, and Australian transplant registries. We reviewed referrals 2010-2015, identifying and characterizing referrals and donors with PBTs. Tumours were classified using World Health Organization (WHO) grading and risk-assessed using Transplant Society of Australia and New Zealand (TSANZ) guidelines. Data linkage was used to determine accuracy of risk assessment at time of referral, and identify any PBT transmission events.
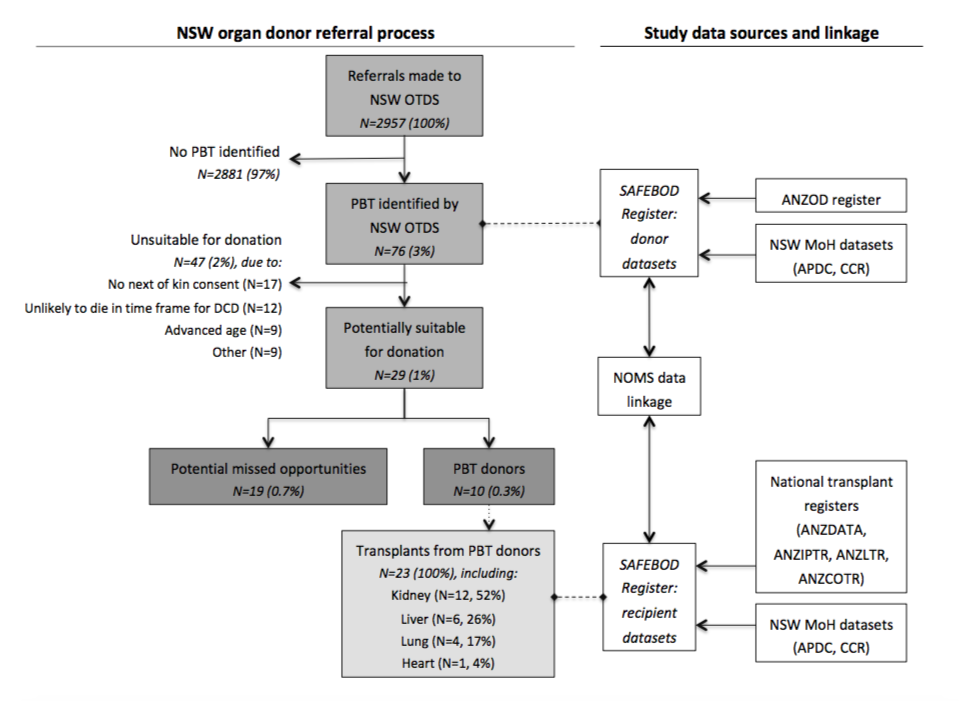
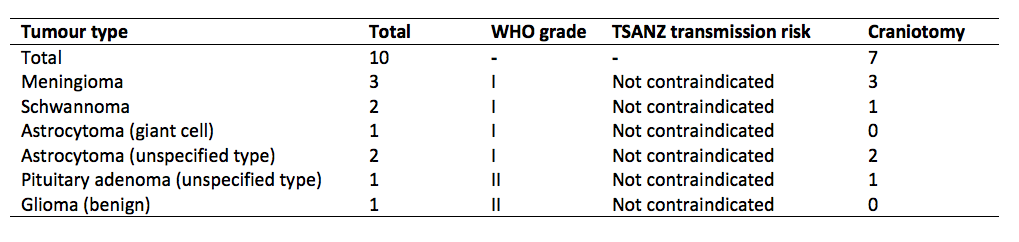
Results: Of 2957 referrals 2010-2015, 76 (3%) had PBT. 44 (58%) of these PBTs were accurately graded at time of referral. Medical reasons other than PBT meant that 47 (62%) referrals were excluded, while 10 (13%) became donors. The remaining 19 (25%) referrals did not proceed to donate, and may represent missed donor opportunities. These referrals were significantly younger (47.7 vs. 58.6 years, p<0.001) and had fewer comorbidities (0.8 vs. 2.1, p<0.001) than referrals overall. WHO-I tumours were most common among PBT referrals (36, 47%) and PBT donors (8, 80%), but WHO-IV tumours predominated among missed opportunities (12, 68%) including glioblastoma multiforme (GBM) (11, 63%). All PBT donors had tumours categorized as ‘not contraindicated’ by TSANZ. No referrals with GBM or ventriculo-peritoneal shunt donated organs. No transmission events occurred after 860 months total follow up of 23 PBT transplant recipients.
Conclusions: There remain opportunities to increase organ donation rates through greater consideration of referrals with PBTs. Risk of PBT transmission must be considered, especially when evaluating referrals with GBM. These risks should be balanced against others in transplantation, including receiving a marginal transplant or remaining on the transplant wait list.
New South Wales Organ and Tissue Donation Service. New South Wales Ministry of Health.
[1] Louis DN, Perry A, Reifenberger G et al. The 2016 World Health Organization classification of tumours of the central nervous system: a summary. Acta Neuropathologica. 2016;131(6):803-20
There are no comments yet...