Epidemiology of Nocardia spp infections in heart transplant recipients at a single center
Hannah Nam1, Scott C. Roberts1, Michael P. Angarone1, Valentina Stosor1.
1Infectious Diseases, Northwestern University Feinberg School of Medicine, Chicago, IL, United States
Introduction: Infection with Nocardia spp is a rare complication after heart transplantation (HT). Risk factors for acquisition, diagnosis, and optimal management strategies in this population are poorly defined. In this retrospective case series, we sought to characterize the epidemiology and outcomes of all patients with Nocardia spp infection in HT recipients at our institution.
Methodology: Patients were included if they received a HT at Northwestern Memorial Hospital and developed subsequent infection with Nocardia spp from January 1, 2011 to December 31, 2018. Summary and comparative statistics were performed.
Results:
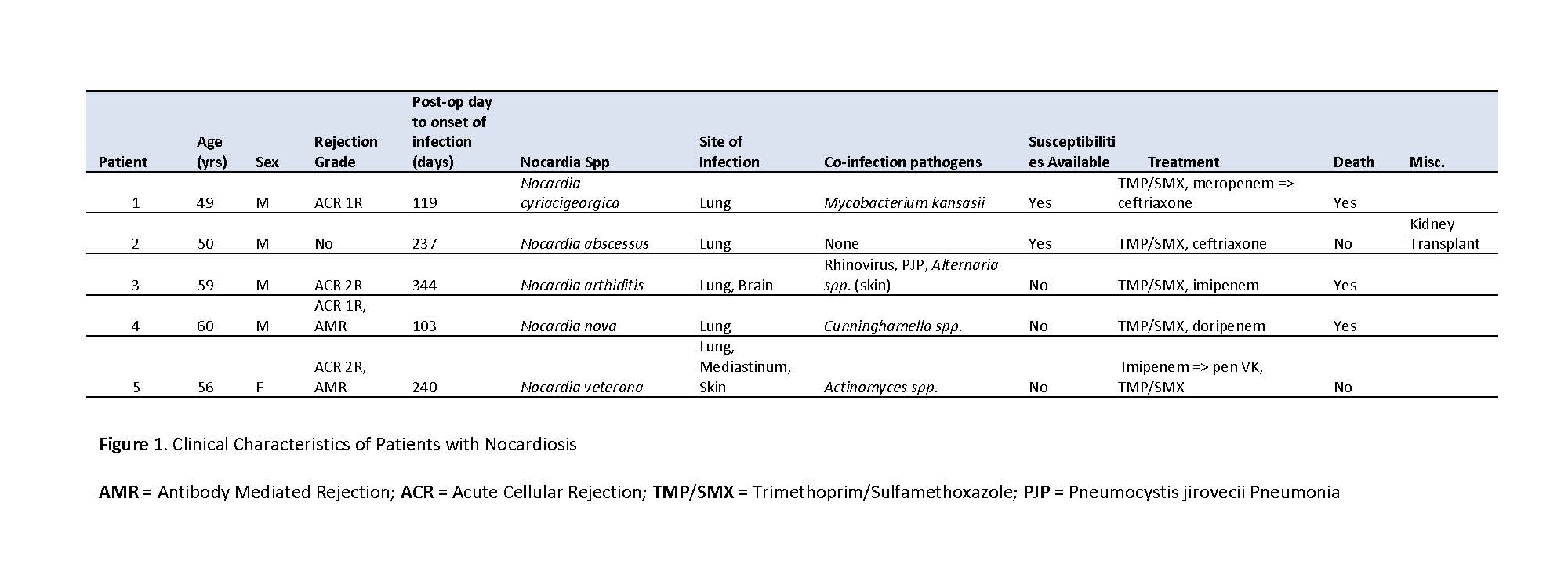
5 patients were identified with Nocardia spp infection after HT (Figure 1). Mean age at diagnosis was 54.8 years. 80% were male (n = 4) and 60% (n = 3) were transplanted for ischemic cardiomyopathy. 80% (n = 4) of recipients received anti-thymocyte globulin for induction immunosuppression. Rejection was identified in 80% (n = 4) of patients preceding microbiologic diagnosis; 60% (n = 3) with cellular rejection and 40% (n = 2) with antibody mediated rejection. 80% (n = 4) received pulse steroids prior to infection.
Diagnosis occurred at a mean of 208.6 days post-HT. 40% (n = 2) of patients were on trimethoprim-sulfamethoxazole (TMP/SMX) prophylaxis at the time of identification. Nocardia spp was a co-pathogen in 80% (n = 4) of cases, with other pathogens including Actinomyces ondontolyticus, Cunninghamella spp, Alternaria spp, and Mycobacterium kansasii. All patients had pulmonary involvement (n=5), while central nervous system (CNS) disease occurred in 20% (n = 1) and skin disease occurred in 20% (n=1). Treatments included dual therapy with TMP/SMX and a cephalosporin or carbapenem in 80% (n = 4) of cases. One patient received carbapenem monotherapy with subsequent clinical cure. Overall crude mortality rate was 60% (n = 3).
Discussion and Conclusion: Lungs are described as the most common site of involvement in Nocardiosis,[1-3] and our results are consistent with this finding. The CNS, skin, and disseminated disease are other presentations, the likelihood of which depends on the individual’s immune status, time to diagnosis, and the virulence of the Nocardia spp. While heart transplant recipients are thought to have potentially better survival when compared to other transplant groups,[2] our mortality rates were still significant at 60%. Interestingly Nocardia spp. was a frequent co-pathogen in this series. Further studies are needed to determine optimal treatment course and duration in Nocardiosis.
[1] Aggarwal D, Garg K, Chander J, Saini V, Janmeja AK. Pulmonary nocardiosis revisited: A case series. Lung India. 2015;32(2):165-168.
[2] Hemmersbach-Miller M, Stout JE, Woodworth MH, Cox GM, Saullo JL. Nocardia infections in the transplanted host. Transpl Infect Dis. 2018;20(4):e12902-e12902.
[3] Steinbrink J, Leavens J, Kauffman CA, Miceli MH. Manifestations and outcomes of nocardia infections: Comparison of immunocompromised and nonimmunocompromised adult patients. Medicine (Baltimore). 2018;97(40):e12436-e12436.
Amrita Dosanjh
2020-09-13 23:58
Thank you for your presentation. Among the patients studied, perhaps you could provide details regarding HRCT. findings.