
Relative survival in kidney transplant recipients with de-novo cancers vs non-transplant cancer patients: A population study 1980-2016
Nicole Louise De La Mata1, Brenda Rosales1, Patrick J. Kelly1, Angela C. Webster1,2.
1Sydney School of Public Health, Faculty of Medicine and Health, University of Sydney, Camperdown, Australia; 2Centre for Renal and Transplant Research, Westmead Hospital, Westmead, Australia
The ReSKiTE study.
Introduction: Advancements in cancer therapies has improved survival in the general population. For kidney recipients with cancer, balancing transplant function with nephrotoxic and other adverse events of cancer therapies may limit survival gains. Relative survival accounts for background mortality and shows excess burden for population subgroups.
Materials & Methods: We aimed to compare relative survival from cancer diagnosis between the general population and kidney recipients in Australia and New Zealand. We included all kidney recipients in 1980-2016 with de-novo cancer post-transplant from the Australian and New Zealand Dialysis and Transplant Registry. Relative survival was estimated using Ederer II in kidney recipients and compared to relative survival estimates from the general population with cancer, both using the general population as reference, adjusting for age, sex, country and calendar year.
Results & Discussion: Of 3,603 kidney recipients, 2,759 had de-novo cancer post-transplant where 1,612 died over 14,181 person-years. There were 201 recipients with colorectal cancer (149 deaths), 185 with lung cancer (160 deaths), 296 with melanoma (153 deaths), 153 with breast cancer (69 deaths) and 179 with prostate cancer (73 deaths).
For all-cause cancers, relative survival was consistently lower among kidney recipients compared to the general population with cancer (Figure 1A). At 5 years post-transplant, the relative survival was 0.54 (95%CI: 0.52-0.56) in kidney recipients, and 0.67 in the general population with cancer in Australia and New Zealand. This indicates an excess of 13% of kidney recipients had died following cancer diagnosis than expected in the general population with cancer.
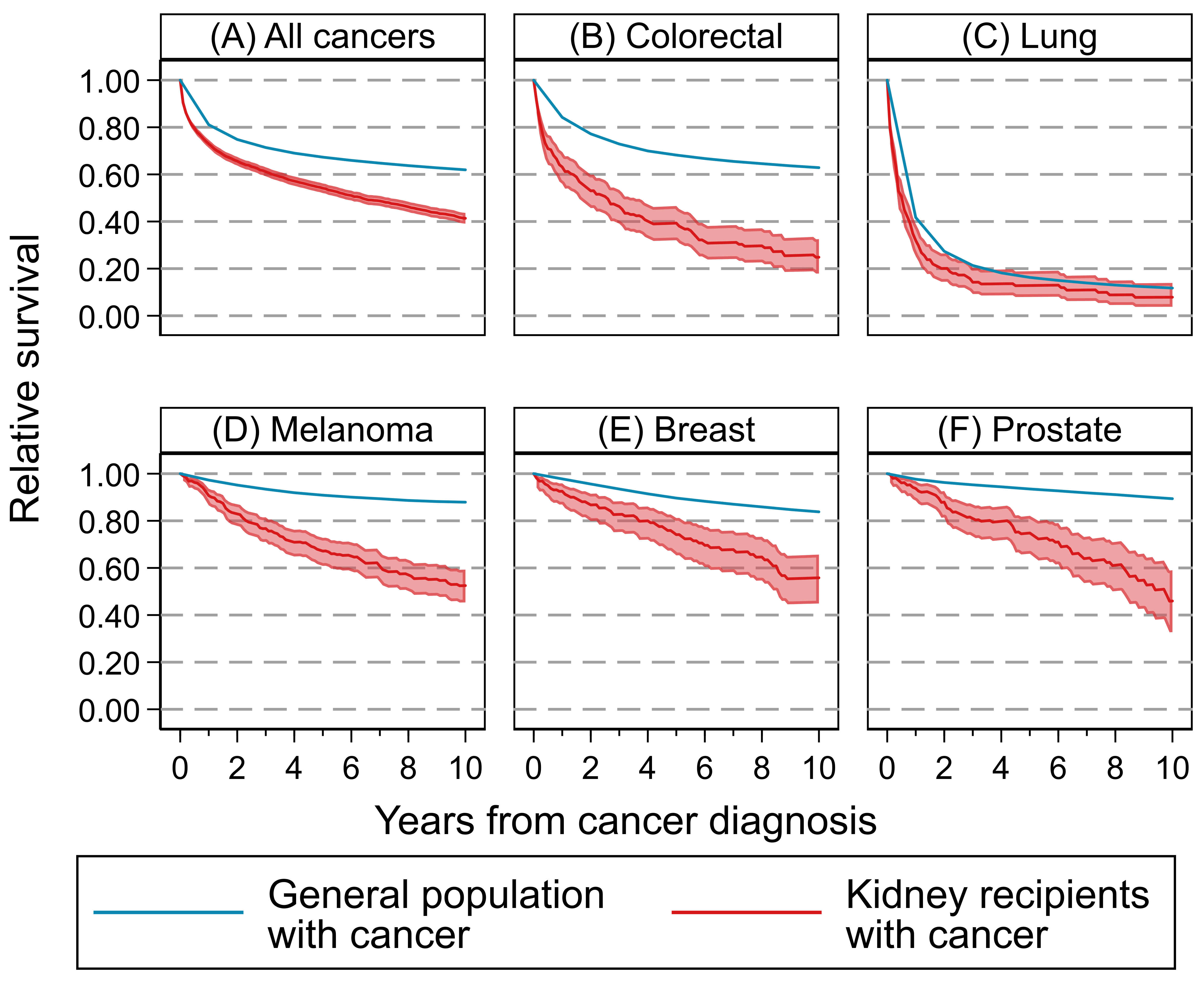
Relative survival remained lower among kidney recipients for most cancer types. The greatest excess was seen in colorectal cancer (0.39 [95%CI: 0.32-0.47] vs 0.68), followed by melanoma (0.67 [95%CI:0.61-0.73] vs 0.91), prostate cancer (0.75 [95%CI:0.66-0.82] vs 0.94) and breast cancer (0.74 [95%CI:0.65-0.81] vs 0.90), but was comparable for lung cancer (0.13 [95%CI:0.08-0.19] vs 0.16) (Figure 1B-F).
Conclusion: Kidney recipients had poorer survival following de-novo cancer diagnosis than expected in the general population, overall and in most cancer types. Reasons for decreased survival may be due to poorer treatment response, drug tolerability or delayed/interrupted treatment delivery.