Renal allograft outcome from hypertensive donor: Comparison between living and deceased donor
Yu Ho Lee1, Sang Ho Lee2, Dong-Wan Chae3, Soo Jin Na Choi4, Seungyeup Han5, Jaeseok Yang6, Curie Ahn7, Hyeon Seok Hwang2.
1Division of Nephrology, Department of Internal Medicine, CHA Bundang Medical Center, CHA University, Seongnam, Korea; 2Division of Nephrology, Department of Internal Medicine, Kyung Hee University, Seoul, Korea; 3Division of Nephrology, Seoul National University Bundang Hospital, Seoul , Korea; 4Department of Surgery, Chonnam National University Medical School, Gwangju, Korea; 5Department of Internal Medicine, Keimyung University School of Medicine, Daegu, Korea; 6Department of Surgery , Seoul National University Hospital, Seoul, Korea; 7Department of Nephrology, Seoul National University Hospital, Seoul, Korea
Korean Organ Transplantation Registry Study.
Introduction: Donor shortage is a serious problem in renal transplantation, and hypertensive living donor is potential candidates to expand donor pool. However, it is not unclear that renal allograft outcome from hypertensive living donor is similar compared to normotensive living donor or deceased donor.
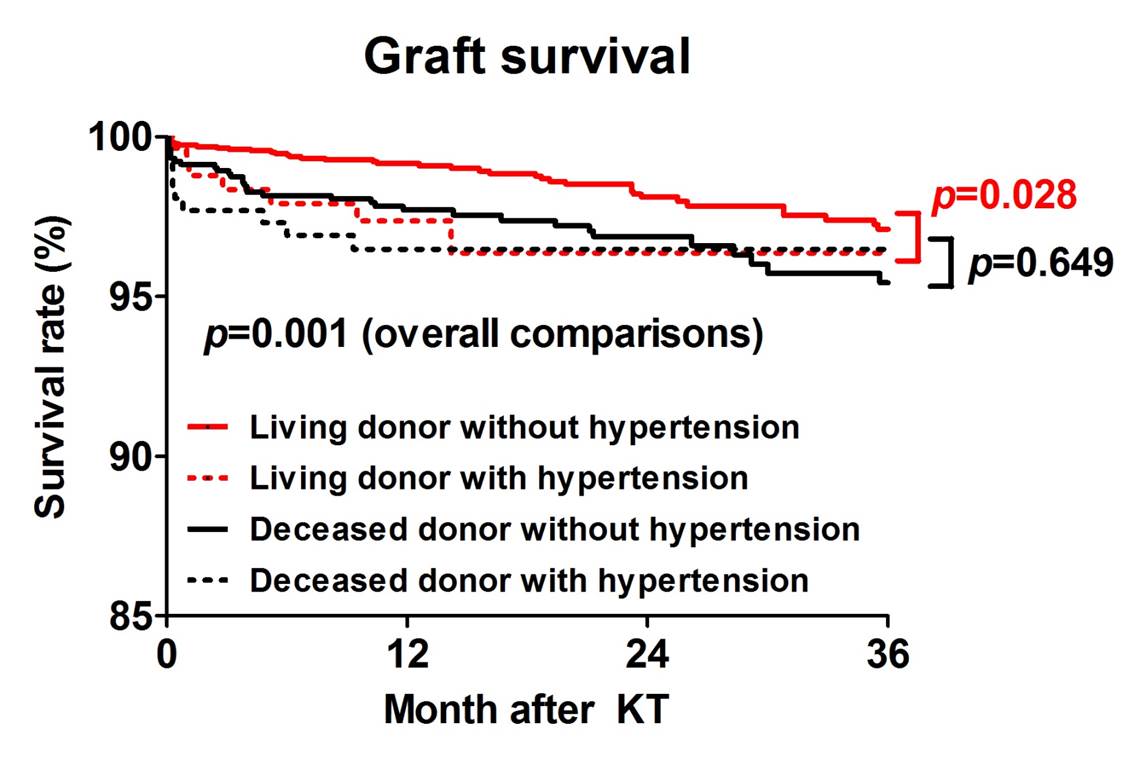
Methods: 4311 renal transplant recipients from the KOTRY database were enrolled from Jul 2014 to Dec 2018. We tried to investigate the renal allograft survival rate and estimated glomerular filtration rate (eGFR) of renal transplant recipients from hypertensive living donor (n = 280), compared to those from living normotensive donor (n = 2723) and deceased donor with or without hypertension (n = 262 and n = 1046, respectively).
Results: Renal transplant recipients from hypertensive living donor exhibited significantly worse death-censored graft survival rate than those from normotensive living donor (p = 0.028). The allograft survival rate was not different between normotensive and hypertensive deceased donors (p = 0.649). In multivariate Cox-regression model, the renal allograft from normotensive donor was significantly associated with better survival rate compared to recipients from normotensive living donor (95% CI 0.18-0.91; p = 0.028). The recipients of hypertensive living donor did not show better graft survival rate compared to those of deceased donor with and without hypertension. The renal allograft from hypertensive donor was associated with lower eGFR than those from normotensive living and deceased donor without hypertension during entire follow up. The presence of donor proteinuria and more than 50 years-old recipients further increased the risk of renal allograft loss in hypertensive living donor transplantation. However, these relationships were not observed in hypertensive deceased donor transplantaion.
Conclusion: Renal allograft from hypertensive living donor had increased the risk of renal allograft loss and associated with lower eGFR.
This study was supported by the Korean Society for Transplantation, and funded by the Research of Korea Centers for Disease Control and Prevention .
[1] Jin DC, Yun SR, Lee SW, Han SW, Kim W, Park J et al. Current characteristics of dialysis therapy in Korea: 2016 registry data focusing on diabetic patients. Kidney research and clinical practice 2018;37(1):20-29
[2] Saran R, Robinson B, Abbott KC, Agodoa LYC, Bragg-Gresham J, Balkrishnan R et al. US Renal Data System 2018 Annual Data Report: Epidemiology of Kidney Disease in the United States. American journal of kidney diseases : the official journal of the National Kidney Foundation 2019;73(3S1):A7-A8
[3] European Renal Best Practice Transplantation Guideline Development G. ERBP Guideline on the Management and Evaluation of the Kidney Donor and Recipient. Nephrology, dialysis, transplantation : official publication of the European Dialysis and Transplant Association - European Renal Association 2013;28 Suppl 2:ii1-71
[4] Lennerling A, Loven C, Dor FJ, Ambagtsheer F, Duerinckx N, Frunza M et al. Living organ donation practices in Europe - results from an online survey. Transplant international : official journal of the European Society for Organ Transplantation 2013;26(2):145-153
[5] Lentine KL, Kasiske BL, Levey AS, Adams PL, Alberu J, Bakr MA et al. KDIGO Clinical Practice Guideline on the Evaluation and Care of Living Kidney Donors. Transplantation 2017;101(8S Suppl 1):S1-S109
[6] Forouzanfar MH, Liu P, Roth GA, Ng M, Biryukov S, Marczak L et al. Global Burden of Hypertension and Systolic Blood Pressure of at Least 110 to 115 mm Hg, 1990-2015. Jama 2017;317(2):165-182
[7] Issa N, Stephany B, Fatica R, Nurko S, Krishnamurthi V, Goldfarb DA et al. Donor factors influencing graft outcomes in live donor kidney transplantation. Transplantation 2007;83(5):593-599
[8] Sofue T, Inui M, Kiyomoto H, Moritoki M, Nishioka S, Nishijima Y et al. Pre-existing arteriosclerotic intimal thickening in living-donor kidneys reflects allograft function. American journal of nephrology 2012;36(2):127-135
[9] Textor SC, Taler SJ, Driscoll N, Larson TS, Gloor J, Griffin M et al. Blood pressure and renal function after kidney donation from hypertensive living donors. Transplantation 2004;78(2):276-282
[10] Yang J, Jeong JC, Lee J, Kim YH, Paik HC, Kim JJ et al. Design and Methods of the Korean Organ Transplantation Registry. Transplantation direct 2017;3(8):e191
[11] Levey AS, Stevens LA, Schmid CH, Zhang YL, Castro AF, 3rd, Feldman HI et al. A new equation to estimate glomerular filtration rate. Annals of internal medicine 2009;150(9):604-612
[12] Hill GS. Hypertensive nephrosclerosis. Current opinion in nephrology and hypertension 2008;17(3):266-270
[13] Naesens M, Kuypers DR, Sarwal M. Calcineurin inhibitor nephrotoxicity. Clinical journal of the American Society of Nephrology : CJASN 2009;4(2):481-508
[14] Rossi AP, Vella JP. Hypertension, living kidney donors, and transplantation: where are we today? Advances in chronic kidney disease 2015;22(2):154-164
[15] Rao PS, Schaubel DE, Guidinger MK, Andreoni KA, Wolfe RA, Merion RM et al. A comprehensive risk quantification score for deceased donor kidneys: the kidney donor risk index. Transplantation 2009;88(2):231-236
[16] Truong LD, Suki WN, Gaber LW, Gaber OA, Khan F. Kidney Donors With Diabetes: Renal Biopsy Findings at Time of Transplantation and Their Significance. Transplantation direct 2019;5(7):e465
There are no comments yet...