The new crescentic incision: A good option for donor nephrectomy
Mehmet A. Haberal1, Mahir Kirnap1, Omar AlShalabi1, Pulat Sultanov1, Aydincan Akdur1, Ebru H. Ayvazoglu Soy1, Sedat Yildirim1, Gokhan Moray1, Zeynep Kayhan2, Adnan Torgay2.
1Transplantation, Baskent University, Ankara, Turkey; 2Anaesthesiology, Baskent University, Ankara, Turkey
Background: Living kidney donation helps to avoid or reduce the time period of dialysis and on waiting lists in patients requiring a new organ. We are think new crescent incision donor nephrectomy to be an effective and less invasive modification of classic open donor nephrectomy (CODN). Our aim was to present our experience at Baskent University Hospitals with the new crescentic open donor nephrectomy technique and compare it to other approaches.
Materials and Methods: 135 patients were retrospectively evaluated and divided into 3 groups (laparoscopic donor nephrectomy (LDN), crescentic incision open donor nephrectomy and CODN) with 45 patients for each group. We assessed: demographic aspects and pre- postoperative evaluation for the three groups. Acute renal graft dysfunction and graft survival rate for first year were also assessed in recipients for the donors.
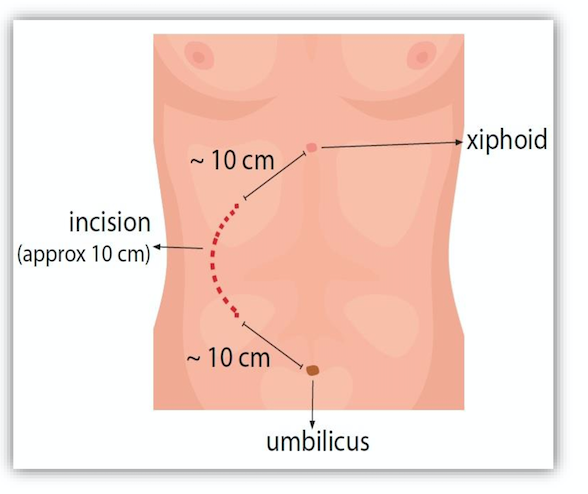
Results: Patients of the CODN group presented higher pain score (p= 0,010), had longer hospital stay (3, 24 vs 3,5 ) and a less quality of life comparing to our new incision. New Crescentic incision group showed less rate and less serious complications (20% vs 24,4%). There was no difference in mean operation duration and warm ischemia between these two groups. Mean operation time (p= 0,016), warm ischemia time (p=˂0,001) were significantly longer in LDN comparing to our new crescentic incision. Pain score, complication rate, hospital stay and quality of life rates were in favor of LDN group (2,2 vs 2,3 , 15,6% vs 20%, 3 vs 3.2 respectively). Our recipient group’s assessment showed similar rates of first year survival and delayed graft dysfunction.
Conclusion: The use of the new crescentic incision is safe, comfortable to the patient, the surgeon and the anesthetist as well during the surgery and postoperative period for the patient.
There are no comments yet...